Reduce
Claims
Costs
Leverage your plan assets and the power of AI to discover, recover, and prevent medical overbilling.










Proud To Partner With





Comprehensive Monitoring
Bluespine reviews EVERY claim to ensure that no potential savings slip through the cracks.
Customized Analysis
We leverage AI to conduct reviews that enforce the specific terms of your individual plan contracts.
Frictionless Recovery
Seamlessly pinpoint claims errors and recover unwarranted charges, without interrupting members or benefits.
Every plan needs its own key
Medical claim analysis unlocks real savings when rulesets are tailored to each employer's specific plan policy.
Your one stop shop for streamlining claims cost containment
Eliminate blind spots and recover losses using one centralized platform.
Visibility
Keep tabs on potential savings across 100% of benefits to enhance budget management and forecasting.

Reporting
Streamline recovery processes with detailed reports and supporting documentation.
.webp)
Automation
Automatically generate customized rule sets to enforce the negotiated terms of your contracts.

Actionable Insights
Gain visibility into potential compliance issues with health benefits, and adjust your plans accordingly.
.webp)
.webp)
Recovery Management
Track Bluespine’s progress on the recovery of erroneous claims from a single dashboard.
.webp)
.webp)
Case Study
Results are based on an analysis of claims provided by a mid-size employer managing 12,000 lives.
Just 4 Steps to Recovery
Start using Bluespine without lifting a finger.
1. Register
Swiftly complete our onboarding process

2. Access to Claims
Introduce us to your TPA or ASO to obtain claims data

3. Analyze Claims
Use the power of AI to identify overbilling

4. Get Reimbursed
Recover your financial losses

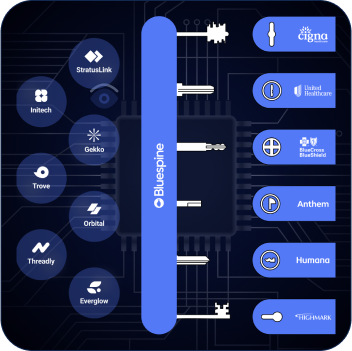
Built for the health insurance ecosystem
Employers
Maximize your healthcare savings, reduce financial risk, and fulfill your fiduciary duties.

Auditors
Scale your auditing capacity to drive revenue growth and unlock new markets.

Brokers
Leverage AI technology to save your clients money, without increasing their costs.

TPAs / ASOs
Differentiate yourself with cutting-edge tech that improves your customers' bottom line.


Enhance your ERISA compliance strategy
Adhere to fiduciary responsibilities
Demonstrate prudent use of plan assets
Responsible plan management
Bluespine can be leveraged by anyone in the employer-sponsored health insurance value chain. Employers typically use the platform to contain their healthcare costs and fulfill their fiduciary obligations. TPAs, brokers and auditors use Bluespine to scale their business and better serve clients in their ecosystem.
TPAs and carriers typically rely on automated solutions for claims adjudication, instead of conducting human reviews. However, most auto-adjudication software relies on static, universal rule sets when scanning for errors, and lacks customization to accommodate the specific plan documents of employers.
Bluespine provides a data driven, AI-powered layer of protection to help claims processors accurately pinpoint overbilling and catch errors that most legacy solutions fail to detect.
Yes, we’ll generate detailed reports with relevant documentation, and wor diectly with your claims processor to ensure maximal recovery from overbilling errors.
We tailor our analysis to the specific terms of your plan documents and leverage a wide range of data sources to maximize our success in error detection. In general, you can expect Bluespine to save you up to 10% of your annual healthcare expenses.
Under the Employee Retirement Income Security Act (ERISA), plan sponsors have a fiduciary responsibility to exercise diligence on behalf of members. Bluespine helps companies leverage their plan assets to reduce healthcare costs for employees, monitor plan performance, and mitigate regulatory risks. Learn more about your fiduciary obligations as a plan sponsor.
Legacy solutions that analyze claims for overbilling typically rely on a static set of rules derived from a single data source, while Bluespine continuously parses and analyzes dynamic information from multiple data sources. We then tailor our rule sets to this data to reliably detect overbilling errors and maximize your healthcare savings.
In addition to achieving pinpoint accuracy in error detection across 100% of claims, Bluespine-generated rule sets can identify recoverable errors that fly under the radar of most competing solutions.
Bluespine is enterprise-ready software and doesn’t require any up front deployment costs. All we need to get started are your plan documents and an intro to your claims processor. No change in member behavior is required for our solution.
Start Saving Money Now